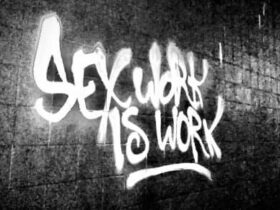
For Sex Workers
By Sex Workers.
The Naked Truth (TNT) is an ethical, Canadian, ‘sex worker’ owned and operated resource, advocacy and advertising website!

Blog
Why I Wrote “Annie Temple’s Business Bible”
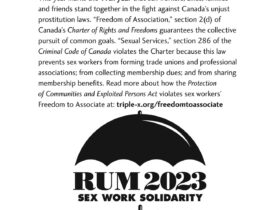
Sex Workers, Allies, Family and Friends March in Anticipation of Ontario Superior Court Charter Rights Decision
Susan Davis: “Powerful lobby attacks all aspects of our lives”
Mandy Goodhandy Rises Again
Problems at the Border? Share your experiences!!
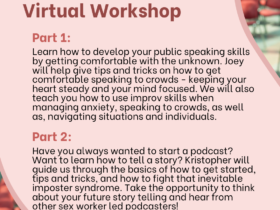
Free bilingual Zoom workshop for sex workers: Speaking Loud & Proud
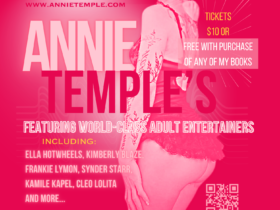
Annie Temple: On Clients, Activism, and her TELL ALL Book
Digital Citizen – Bill C-11
A Review of the Fancentro Adult Content Platform
Press Release: Canada’s Blood Donation Ban for Selling Sexual Services
Call For Presentations (CFP) “Beyond the Interface: Critical Perspectives of Sex Work and Sextech
Problems at the Border? Share your experiences!!
Free bilingual Zoom workshop for sex workers: Speaking Loud & Proud
Annie Temple: On Clients, Activism, and her TELL ALL Book
Free bilingual Zoom workshop for sex workers: Speaking Loud & Proud
Press Release: Canada’s Blood Donation Ban for Selling Sexual Services
Digital Citizen – Bill C-11
Press Release: Canada’s Blood Donation Ban for Selling Sexual Services
“I wouldn’t call the cops if was being bashed to Death”
Bill S-203 – Susan Davis Witness Testimony (16:32)
The Naked Truth (TNT) is an advocacy, resource and adult classifieds website
Our mandate is to support our community in finding connections and business solutions that promote sex worker control of our work!!
Providers
Please support TNT by posting ads and telling your friends about our site! Give us feedback. Ads are free! They link to your free profile which you can use to prmote yourself anywhere you like!
Clients
Please support TNT by checking out our ads first and letting providers know if you found them through our site.
We sincerely appreciate your support!!!
Are you looking for information about your work? Need to be connected to supports?
Check out Trade Secrets – Occupational Health and Safety for Sex work
If you would like to find organizations or support in your area please check out the resources below

Who We Are
The Naked Truth is a media based social enterprise. We work to improve access to information about the sex workers rights movement, create a mechanism for communicating about enforcement against our community, create an affordable advertising platform which encompasses all forms of sex work, ensure people have the tools to make safe decisions about their work and to communicate information about dangerous or problematic clients to our community. We also work to keep our community up to date on the global sex workers rights movement and make sure people know when decisions are being made by government which could impact our lives, safety and ability to work!! We want to ensure your voice and experiences are included in the movement!